Medical necessity of “place of service”
Just when I think we’ve heard it all, our insurance company throws another indignity at us.
Wesley’s current treatment regime is mostly at-home, though (to oversimplify) he has a monthly spinal (LP) for which he’s sedated, during which they draw a cerebrospinal fluid sample for testing and administer a spinal dose of methotrexate. Every third month, they also administer vincristine. During each of these monthly procedures his port is accessed for labs as well as fluids, so he’s always on IV.

For months now, Wes has been carrying a cold – the common coronavirus, it turned out – and while his symptoms have been mild lately, he hasn’t ever quite been able to shake it. A couple of months back, this lead to 6 or 7 ER visits in a short period of time due to fever, each visit itself posing a risk of further infection while not providing much relief besides an opportunity to check his blood counts. After a number of these visits they finally did an Immunoglobulin G (IGG) test, which were very low. With low IGG he’s struggling to recover from this virus, while remaining more susceptible to additional infections.
As a result, they prescribed a series of IVIG transfusions to recharge his IGG. This process is a specific type of blood product transfusion during which they administer a cocktail of IGG antibodies compounded from over a dozen donors to give the recipient the broadest possible sample of antibodies to rebuild their immune system.
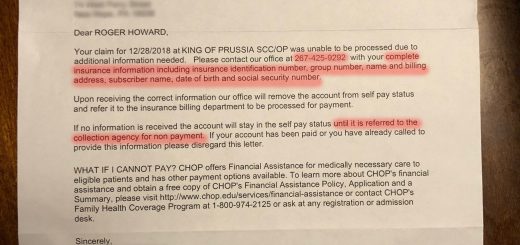
A couple of weeks ago we were notified by our oncology team that our insurance company had initially rejected the claim for the first treatment – after it was performed – and will not approve further treatments as currently planned. While their objection was classified under “not medically necessary”, it turns out the real issue is “place of service” – meaning, they don’t want us to receive this treatment at our normal outpatient clinic, from the oncology team that has handled his care and treatment for more than a year now.
Read that again – this isn’t an objection to the treatment; this isn’t the insurance company flagging a treatment as not medically necessary. This is an insurance company now deciding who gets to perform this treatment – in spite of this being a Tier 1 provider within our network, in spite of the expertise of this team, and – importantly – in spite of the fact that this treatment will normally be administered during an existing appointment while other treatments are also being given.
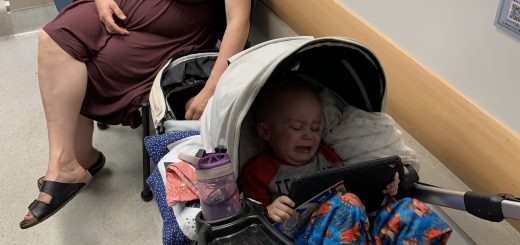
Our son isn’t even four years old. Every treatment is traumatic. He knows his nurses and doctors, and has built up an incredible degree of trust with them, and it’s still difficult, and heart-wrenching. We’ve also seen how poorly equipped many non-pediatric providers are at dealing with the needs of children, let alone non-oncology providers dealing with the needs of cancer patients. This treatment, like all others he receives, requires a specialists approach – we’re not even allowed to go to our regular pediatrician for checkups.
Crucially, this also means an unnecessary port access by strangers instead of piggybacking on an existing appointment with a port access by his trusted team. One extra trauma a month, and additional risk of secondary infections – both from the port access and from a visit to a lowest-bid facility not catering to the immune issues of a kid with cancer. This is unconscionable, and being done over the objections of his doctors.
So what does this mean? We have no idea. Our hospital appealed; our doctors appealed, and even had a conference with the insurance company’s “doctor”, who refused to budge.
Yet, here we are – tomorrow he’s still scheduled for treatment as originally planned because no one can tell us what we’re supposed to do. Do we go forward with the planned treatment knowing full well our insurance company has said they won’t pay, leaving us with a likely enormous bill to pay out of pocket? Do we cancel, knowing how much he needs this treatment? Do we go somewhere else, and if so how?
I escalated this with our oncology team as I’ve asked all these questions and no one can tell us the answer – how to safely receive the treatment he needs without delays and without yet another financial burden we can’t afford?
We are still waiting for answers, with less than 24 hours to go.

Might it be possible to contact your congressional representative and/or local newspaper journalist to request intervention to advocate on Wes’ behalf? Perhaps shinning the harsh light of truth might persuade the insurance CEOs to stop the obstructionist bs and place your child’s best interests first.
Chana Ham-Rosebrock 2020-03-03 at 12:29 pm. Corrected version:
My gut reaction, over this screaming in my head about what you must be going through, is just do it and I’ll send money and hopefully other people will too. Of course I can’t give you the right answer and whatever you choose will be the right answer. My heart goes out to your entire family.
My gut reaction, over this screaming in my head that what you must be going through oh, it’s just do it and I’ll send money and hopefully other people will too. Of course I can give you the right answer and whatever you choose will be the right answer. My heart goes out to your entire family.
I am so sorry Roger! What an appalling situation. It is so important that Wesley receives his treatment in the most least invasive approach as possible. I am so sorry the insurance company is putting their bottom line before the health and well being of their insured little person. My heart goes out to you and your family. This whole process is hard enough without the extra pressures and added frustrations from your insurance company!