Our CHOP billing nightmare continues
When we were first admitted to CHOP back in October, 2018, we were introduced to a variety of specialists who’d be our advocates along the long, complicated path ahead. Doctors and nurses featured heavily, but we’d also come to find how essential social workers, child life specialists, and financial liaisons could be.
Our financial liaison introduced herself early on – within the first week – and told us she’d take care of absolutely everything related to insurance, billing, and the financial impacts of leukemia treatment. Whereas our social worker told us about the incredible Medicaid program for kids like Wes in Pennsylvania, our financial liaison – I’ll call her “S” for short – actually filled out all the paperwork and saw it through to approval. She wanted to know about any strange bills we received, and even went as far as to tell me that if we had *any* problems at the hospital we should simply call her and she would make sure the right person got informed, or yelled at. We seemed like we were in good hands.
During the first few months we were in a deep haze, but had every assurance from “S” things were on track. There were a few signs early on she wasn’t as organized as she wanted us to believe – a few minor dropped balls and lack of follow up when she promised, but nothing alarming. Mostly, she wasn’t communicating consistently – failing to call me back when promised – but when we did speak, she always gave me the impression that everything was being handled. Our Medicaid was approved, though it took her 3 or 4 weeks of emails and voicemails checking in before she finally responded to tell me so. Everything seemed to be good.
During those early months we received many bills for costs that should be covered by Medicaid, but she insisted this was just the three systems – hospital, primary insurance, and Medicaid – all getting sync’ed up, and that eventually it would all be reconciled. She insisted we shouldn’t pay any of the bills, as it would only complicate getting reimbursed later, and in any case it didn’t matter as the hospital would never send us to collections and destroy our credit, one of my biggest fears financially.
Medicaid was approved before end of 2018, but through early 2019 we continued to receive bills. Some alarmingly big. All confusing. But, when I could get ahold of her, “S” always said the same thing – don’t pay them, it’s just crossed-wires, it would all be covered. We’d eventually get our balance due down to $0.
I reached out to her on February 6, 2019 again, still believing all was well, but starting to get annoyed. Every week I’d have a stack of bills from CHOP an inch thick – I’d read through every one, making sure I wasn’t missing anything, but it was enormously stressful. Still, I knew our insurance policy covered it – and if the first one didn’t for some reason, the secondary (Medicaid) would. And not wanting to screw things up further, I resisted the urge to start paying just in case, lest I paint myself into a corner and have to fight for every reimbursement. Also, we were in the thick of frontline treatment, and a pregnancy, so I gave it time, but eventually reached out again:
February 6, 2019
Hi “S”,
Can you double-check with hospital/physician billing that everything is/has been submitted through both our primary and secondary insurance now? I’ve received a few bills still from CHOP which I think should be going through our secondary insurance; I don’t want to risk collections or credit problems so i want to make sure everything has been sorted out with our Medicaid coverage/etc.
After a week, I followed up with a call, which lead to a voicemail. All I needed was an update and an assurance that all the bills were being properly handled by CHOP, our primary insurance, and our secondary (Medicaid).
Another few weeks went by, some of the hardest during frontline treatment, as well as the final month of Stephanie’s pregnancy, so we had a lot going on. Again, I left more voicemails asking if I could come by, since we were frequently in-patient, probably 100 yards from her desk. No reply. I sent my last email and voicemail to her March 14:
March 14, 2019
Hi “S”,
I never heard from you regarding this but I’m still ocassionally receiving bills from CHOP – I’ve tried calling the billing department but I was told to wait and they should be cleared, but we still seem to be getting them. Can you please confirm with CHOP billing that all our past bills are cleared and future bills are submitted through our secondary insurance?
As hectic as this time was, and as many other terrible things as we had going on, this was starting to bubble up as a significant concern. We were getting stacks of bills, and my financial coordinator had now been completely non-responsive for over six weeks.
That week, I reached out the best person I could think of – our social worker. She’d shown herself, time and again, to be caring and resourceful and we hoped she could help. I called her, talked her through the background, the enormous stress our financial uncertainty was causing, and my complete puzzlement at how our financial liaison had just disappeared on us. She promised to find out what she could.
The next day she called me, and laid out what she could – she made it clear there was a huge mess in billing, that they were still trying to wrap their arms around it, and that they hadn’t yet realized we were impacted. She promised a call from that department to bring me up to speed, as she wasn’t able to speak for them or really provide any more detail, but that she’d make sure they followed up and connected me with people who could help.
That afternoon I got a call from another person in billing, “M”. She briefed me as best she could without compromising any personnel privacy, but from what I gathered “S” was a former co-worker of hers, who had recently left the hospital and, with her departure, an apparently enormous mess of billing problems that heretofore had somehow not been visible to her superiors. Her sudden departure created a void in the department that alone would have increased workloads, but combined with what must have been months of billing problems across many different families, they were scrambling hard to even figure out what was what. This was not reassuring in the moment, but she promised they would get to the bottom. One thing I asked specifically about was whether CHOP was going to take full responsibility for financial liability – that whatever came of this situation, I should owe nothing – that any unpaid bills would be, worst case, written off by CHOP. She repeatedly, and unambiguously, stressed this was the case – that the mistakes were theirs, and they would deal with it and make it right.
I, of course, asked how one person could create such a mess, why there wasn’t any oversight, and for the matter why it took more than six weeks of me contacting them – at least several of which occurred after she departed – with no follow up. Why wasn’t a supervisor checking her voicemails and emails after she left? Why did it take me escalating with my social worker to get any contact? She never had an answer for this.
Beginning in mid March, 2019, I was in regular contact with “M” as my new billing liaison. She repeatedly assured me that they were working through the backlog, that there was nothing I could or should do to help, and that eventually it would all get sorted out. In this period, I still received confusing bills and statements, but I begin to see what appeared to be progress. At one point I even received a refund. If you’ve ever tried to decipher medical billing I don’t have to tell you how impossible it was to actually figure out what was going on, but something was happening.
At some point in this process, “M” also gave me the direct line to “D”, the billing supervisor, in case I needed to escalate. At some point in May, I believe, I started reaching out to “D” to get an update, as the billing issues seemed still not fully resolved – I was still getting confusing, conflicting, and overlapping statements, none of which showed what I expected to see: a $0 balance due.
In May, I called, and then emailed “M” again, leaving her the following:
May 7, 2019
Hi “M”,
This is patient Wesley Howard’s father; we spoke about the billing issues you were looking into for me. We are still getting bills from CHOP which we shouldn’t owe; I tried calling “D” last week and haven’t received any contact back. I’d love to get an update on the status of our accounts with CHOP and why we are still getting bills which should be fully covered by our primary or secondary insurance.
And two days later she replied:
May 9, 2019
Hi Mr. Howard ,
I will reach out to “D”/ Billing department so they can adjust this.
Suffice it to say, I never heard back from either.
On June 25, 2019, I reached out to “D” directly via phone and then email:
June 25, 2019
Hi “D”,
I wanted to see if you can make sure we don’t have any balance owed to CHOP – as we’ve discussed in the past there seemed to have been some billing problems which you investigated, and it looked like it was all resolved. However, we still occasionally get bills as well as a recent credit (a check made out to us), so we’re really unsure if we owe anything, and if so why. We have both primary and secondary (PAMA) insurance. Can you check and make sure we don’t have an outstanding balance?
Also, I’m not sure if you can help with this, but we’ve been getting claims rejection letters sometimes from our primary insurance; most of the time they don’t seem to make any sense. For instance, we recently received one rejecting a treatment (code 96450), which appears to be a totally routine part of my son’s treatment. They’ve also been rejecting various pharmaceuticals prescribed by or administered by our doctors. Should we be concerned with this?
Thanks for any help you can provide
Roger Howard
Father of Wesley Howard
She replied ten minutes later, asking me to confirm Wesley’s date of birth. I replied less than five minutes later:
June 25, 2019
Hi, thanks for the quick reply. My child’s name is Wesley Howard, dob 5/25/2016. Thanks!
Then… nothing again. No response, no follow up.
This week, out of the blue Stephanie received a notification on the MyCHOP portal that we had balance due, though the last time we looked there was none, and immediately asked me to look into it. I logged in, and found the system is now showing we have a balance, with no explanation of the charges – when I click the “Charges” link on the billing portal, I get a blank page. The site helpfully offers to let me setup a payment plan, for this bill which they can’t explain, and which I should not owe. At this point, I don’t trust or believe anything these systems say, so again I reach out to “D”. I forward her our last thread, in June when I asked her to confirm I have no balance due – and which she never followed up on.
The next day she replies that while this is a “physician billing” issue, and she only handles “hospital billing”, but that she’d reach out to someone to make sure they had the correct insurance information for us. Ignoring that she, nor any of her predecessors in prior conversations, had ever disclaimed responsibility for sorting out our “physician billing” issues, this was at least something. I decided to wait a few days – though it turns out I didn’t need to.
The next day – yesterday, in fact – Stephanie opens our mail and finds the following letter from CHOP:
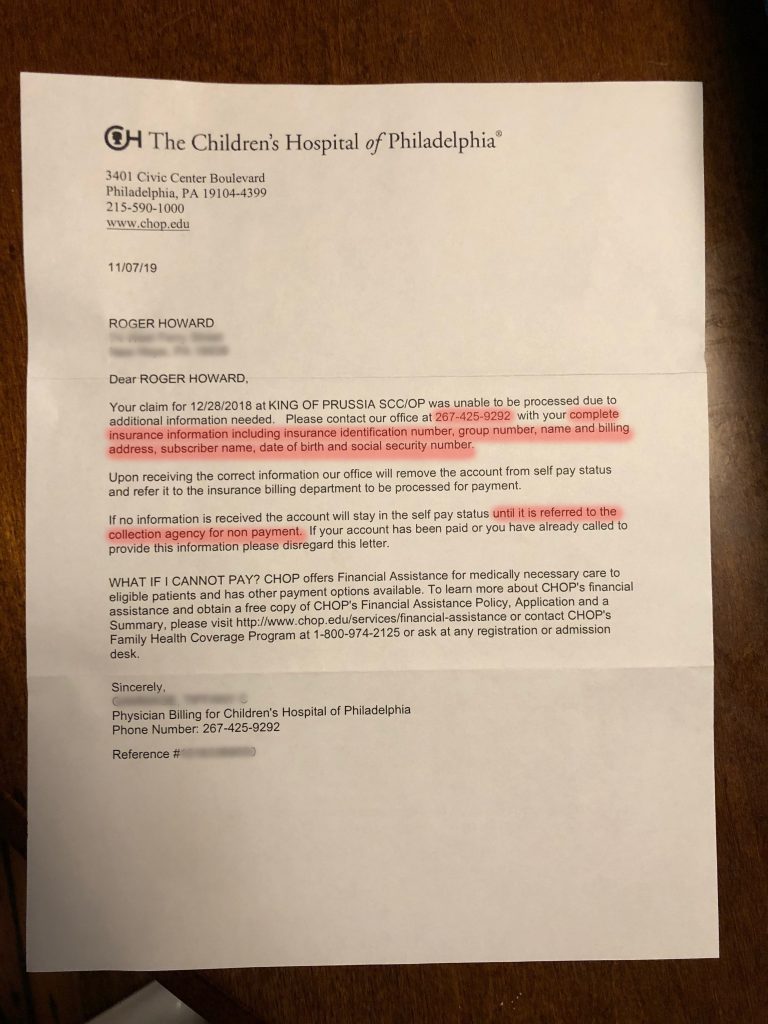
I highlighted a few salient sections in this letter:
- The phone number provided is immediately picked up by a robo-operator, with no announcement of what department I’ve reached or whether I’m even calling CHOP, and says simply “Please enter your ID number”. I tried every ID number I could think of, but none let me through – once I entered an ID number, it asked asked for a pin. What pin? I’m calling the phone number they instruct me to call to sort this out, and I can’t even get through, and no attempt to contact the operator – dialing “0”, saying “operator”, etc., got me past the robo-message.
- The letter is demanding insurance information, but of course we’ve had hundreds upon hundreds of interactions with CHOP before and after the date of the supposed claim this is in regards to – December 28, 2018 – and our insurance and contact information hasn’t changed at all during the entirety of Wesley’s treatment. They have all the information I can possibly provide. We still receive treatment at that facility regularly.
- And finally, the real outrage – threatening to send this to collections. They have made zero effort to collection this past-due bill, which we don’t owe. I answer ever email, every phone call, and every physical mail from CHOP. We’ve been repeatedly told not to pay any bills as they were all in error, and should have been submitted through our primary and secondary insurance. And yet here we are, CHOP threatening to ruin my financial stability by reporting me to collections.
I’m a contractor with a stellar credit score which we both work very hard to maintain, because we have little financial stability besides it: I pay for insurance out of pocket as I receive no benefits from my clients, and without strong credit I’d be in ruins. And yet here we stand, our otherwise amazing hospital, threatening to destroy the foundation of my tenuous financial security, over their own mistakes which they’ve had more than 6 months to correct.
I’m stunned, angry, and completely unsurprised. And, as I always tell people, we’re actually the lucky ones. This process has drained our savings, but we have some left. It’s cost us enormously, but we know so many families even worse off. But that doesn’t mean it’s right, or acceptable. The amount of stress this experience has added to a family already far beyond any reasonable ration of stress is incalculable. It’s immoral, and violates the spirit, and letter, of the Hippocratic Oath. This process has done us harm, adding enormous stress, sleeplessness, and worry to an already devastating experience, and threatens to do additional, lasting harm by reporting me to collections, ruining my credit score for years, causing every aspect of our financial life to be more expensive and more difficult, through zero fault of our own.
I’m at a loss for how to proceed, other than writing about this publicly in greater detail than I have before. It seems that often this is the only way to get any attention on institutional failures like this.
All I want is a final, written guarantee that we owe nothing between the time of diagnosis and now, that they will never send me to collections for anything from that period, and that this was their mistake they are willing to take responsibility for. How hard can this be, to accept that we paid our outrageously high premiums, our enormous out of pocket maximums, and our taxes, and only expect the hospital – and its physicians – to charge us what we owe, which today is $0.